photo by Michelle Rose Photo
New motherhood is isolating. It’s hours and hours spent alone with a newborn. Who is quite often crying. Or nursing. Or being held. Or needing to be held. Or played with. Or bathed. Or any combination of a million tiny things. Yes, there are those moments where things are amazing and sunshine and rainbows shoot out their butt and you both can’t contain your joy as fits of giggles and a thousand iPhone photos are had.
But those other moments? Those darker ones when you feel so alone and overwhelmed are there too. In this social media culture where we share the most perfect and edit moments of life we can too easily forget that those moments are simply that. Moments. Often staged and manipulated for likes and engagement. I admit I’ve done that too.
My lowest point thus far came around when Baby P was 8weeks old. We’d been out far too long that day but I had been enjoying myself talking to other adults and being charming (or so I hope I’d come off that way!). I even wore lipstick for the occasion. By the time we got home, P had been crying hysterically for over an hour with no end in site. Another 2 hours later and I was losing it. I hadn’t eaten dinner, desperately needed a shower (postpartum sweat + spit up is a gross combination) and was feeling defeated in a way I hadn’t yet felt. I agonized over finding and sterilizing a pacifier in the hopes that this small piece of plastic would be the secret to cure what ailed him.
When my husband eventually returned home (after a text that both the baby and I would be in tears when he returned) I begged him to take the baby for 5 mins so I could shower. The desperation was real. He asked why I hadn’t come home sooner and the next time I shouldn’t do so much. Daggers shot out my teary eyes. I felt like I was failing. Failing at everything mom related. I just wanted to hand baby over and melt down the shower drain.
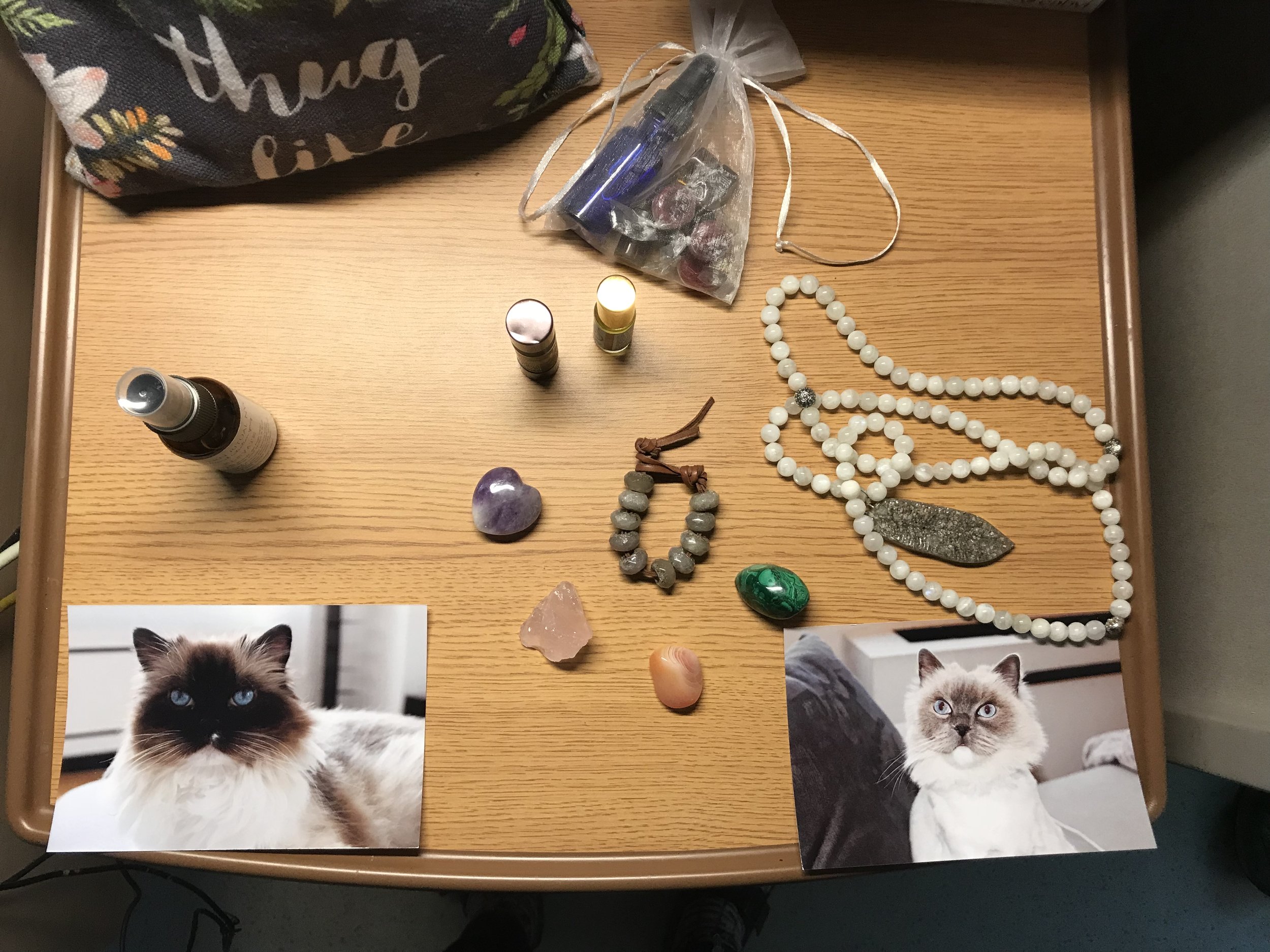
raw, red and real.
A long cry in the shower and I stepped out to start the cycle of bouncing, rocking, swaying and simultaneously shushing the baby to sleep alone in our dark room.
Once I finally admitted to myself that I just may have a colicky baby, it got better the next day. And even better the next day. Sometimes I wonder if it was reaching this breaking point and surrendering that cleared the way or if his colossal meltdown was a developmental shift that lead to more ease. Who knows. I’m just thankful for it.
I’m also thankful for the community of friends, doulas and mom friends who are with me- via text, Instagram and phone calls. Those check ins and “me too”s help more than you may realize. To not feel so alone and to normalize these feelings is so helpful. The question of “is this hormonal?” Or questioning if it is indeed a postpartum mood disorder can be complex and confusing. What is normal after your life has been completely turned on it’s head is hard to distinguish.
Having support and a listening ear can go a long way. Build a supportive nest of helpers before your baby arrives. Connect with other expecting people who you can text at 2am when you’re up for yet another feeding session. I’m lucky to have so many friends having babies at the same time that I had Baby P that there was no shortage of text friends when I need to vent, cry, laugh, share or just simply know I’m not alone.
You’re not alone, mama. I hear you. I see you. I’m here with you.
If you do feel like you may have a postpartum mood disorder or aren’t sure, please take the Edinburgh Scale, speak to a professional (your care provider, a therapist) and/ or seek out a support group. If you’re in NYC, The Motherhood Center and The Seleni Institute are wonderful resources. 1 out of 5 new parents experience some sort of postpartum mood disorder within the first year after giving birth. There IS help available.